Despite refinement in operative technique (particularly laparoscopic surgery), instrumentation, and the never-ending quest for adhesion-prevention products, postoperative adhesions remain a major cause of pain, infertility, and bowel obstruction. Postoperative adhesions are, quite simply, a fact of life in the world of abdominal and pelvic surgery.
Post-surgical adhesions develop immediately after pelvic and abdominal surgery. Data suggests that 60 to 90% of patients will develop adhesions following non-gynecologic abdominal surgery and 55 to 100% develop adhesions following gynecologic surgery. These adhesions become critically important from the standpoint of reproductive potential if the woman is in her reproductive years. Additionally, adhesions are often the cause of pelvic pain, abnormalities of bowel function, and small bowel obstruction.
Every gynecologic surgeon must consider the potential for formation of adhesions after surgery and take intraoperative steps to minimize that probability. The surgeon must have a thorough understanding of 1) how and why adhesions form, 2) what surgical circumstances worsen the chances of adhesion formation, and 3) which pelvic organs are more prone to significant adhesions. This knowledge is invaluable during surgery when decisions are made in a split-second.
Types of Adhesions
Postoperative adhesions come in many varieties. De novo or new adhesions form at a site where none existed before a surgical procedure was performed. Examples include adhesions forming on a myomectomy incision (where a fibroid was removed from the uterus) or an ovarian incision for the removal of a benign ovarian mass. De novo adhesions may also develop in areas of the pelvis where no surgery was done.
Recurrent adhesions develop in areas where adhesions already existed and were surgically treated. They simply `come back`, sometimes worse than before they were treated.
Adhesions can be categorized into 3 primary types: filmy (vascular and avascular), dense (vascular and avascular), and cohesive. The underlying pathophysiology of all three, however, is similar.
Filmy adhesions loosely connect one pelvic organ to another. They are translucent, like an extremely thin sheet of paper. They may have visible blood vessels within the adhesion (vascular) or not (avascular). Avascular filmy adhesions are the least likely to recur after they have been removed. Blood vessels within the adhesion bleed when the adhesion is cut and the bleeding is associated with a higher chance of recurrence.
Dense adhesions also connect organs (that are not meant to be connected), but they are thick, flesh-colored, and opaque. Most contain blood vessels. When these adhesions are cut (lysed) or removed (excised), bleeding usually occurs. The combination of thick adhesions and bleeding results in a very high incidence of these adhesions recurring.
Cohesive adhesions literally `glue` one organ to another. An ovary may, for example, be stuck to the uterus with cohesive adhesions that make it appear that the ovary is glued in place. There is no space between the two organs. Blood vessels abound in the area where they are stuck together. The two organs can be surgically separated, but the chances of the two re-adhering is extremely high. Cohesive adhesions are the most technically difficult (and potentially dangerous) to treat and are the most likely to recur.
The ovaries, fallopian tubes, and the surface of the uterus are the most likely organs to be involved with postoperative adhesions. In addition, different surfaces (medial, lateral, anterior, posterior) of the same organ carry different risks of forming adhesions.
How to pelvic adhesions form?
The peritoneum is the lining of the abdominal and pelvic cavities. It is a very thin, translucent, delicate layer of tissue comparable to a sack in which the pelvic organs live. The peritoneum is composed of multiple layers. The mesothelium is the innermost layer, a layer of connective tissue which contains the blood vessels, and a basement membrane. When the peritoneum is injured (which is inevitable during surgery), there is an inflammatory response.
During the initial phase of this inflammatory response, inflammatory mediators and histamine are released from mast cells and leukocytes. Capillaries located within the connective tissue dilate and the wall of the capillary becomes more permeable (leaky). This allows leukocytes, red blood cells and platelets to become concentrated at the site of the surgical injury. This becomes a fibrinous exudate at the site of injury. Multiple factors such as prostaglandins, lymphokines, bradykinin, serotonin, transforming growth factor and other chemotactic agents are present within this material. The exudate congeals to form fibrin, which protects the injured area.
At this point the fibrinous exudate may be broken down and cleared by a process known as fibrinolysis. If this happens, adhesions are minimal. Under normal circumstances plasmin breaks down exudated fibrin. If this does not occur, the fibrinous exudate is converted into an organized adhesion and collagen fibers are deposited in the area. Following this, blood vessels begin to grow into the fibrin/collagen matrix and an adhesion is formed.
This process begins a few hours after surgery and is completed within seven days. In general, at seven days the volume of adhesions is fixed (unless there is more tissue damage from infection, bleeding, etc). Over the next few months, the adhesions may become thicker and more vascular as blood vessels grow into the area.
For decades, biomedical companies have developed and tested numerous products meant to prevent or minimize adhesion formation after gyn laparoscopic surgery. It has been a frustrating, expensive, and fruitless endeavor. Despite these efforts, only one product has been FDA approved for this purpose, and its efficacy is minimal, at best. Gynecologists often use some products `off label` which have not been FDA approved, but none of these have been shown to be of any significant value in preventing adhesions. Some may actually worsen the problem. In short, there is no currently-available, FDA approved product that has been proven in prospective, randomized, controlled studies to be effective in minimizing adhesion formation/reformation after gyn laparoscopic surgery in any meaningful way. If a product has not been proven nor FDA approved, there is probably a good reason.
What is left for us to do? Based on my experience with over 20 clinical research trials of adhesion-prevention products, over 250 second-look surgeries to evaluate postoperative adhesions, and over 8,000 laparoscopic surgeries I have come to the following conclusions:
Knowing when not to operate is often the most critical decision we can make. Some situations are simply not amenable to surgical correction (from an adhesion standpoint), particularly in the infertile patient. (see photos below) Since IVF can be successful regardless of pelvic/ovarian/tubal adhesions, there may be no reason to undergo adhesion surgery (it is risky and the adhesions usually recur). When pelvic adhesions may be causing pain (and fertility is not an issue), if they are dense, vascular, and/or cohesive, surgery is very unlikely to eliminate the adhesions and may, in fact, worsen them.
Every laparoscopy for pelvic adhesions must have a very clear goal that is attainable. The character and location of the adhesions in question largely determine what a reasonable outcome will be. What are your goals of the surgery? They should be discussed at some length with your surgeon before you get into the operating room.
When treating pelvic adhesions but preserving the uterus, tubes, and/or ovaries, laparoscopic surgery is simply better in the hands of a trained and experienced gynecologic surgeon than laparotomy (open surgery).
Anytime you are having laparoscopic pelvic surgery for a benign (non-cancerous) condition, insist that your surgeon take photographs of your pelvis before and after the surgery. These photos can be invaluable to your new gynecologist years later. They are infinitely superior to a written report.
For treatment of pelvic adhesions (and most other routine gynecologic surgery), robotic surgery has not been shown to offer any advantages over traditional laparoscopy techniques. It just takes longer, has more incisions, and costs more.
If you are undergoing routine extirpative surgery (removing the uterus and ovaries), postoperative adhesions are usually not a clinical concern are unlikely to be a problem for you in the future unless you suffer surgical complications.
Just because you have pelvic adhesions does not mean they are the source of your problems. Many if not most pelvic adhesions are of no clinical significance.
The surgeon`s experience, knowledge of how, why, and under what circumstances adhesions are most likely to form/reform, and technical skill are the most important factors to consider in optimizing your surgical outcome.
See below for surgical photographs of pelvic adhesions.
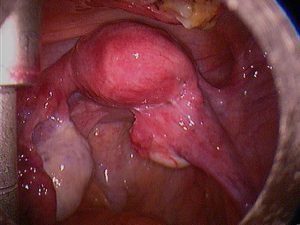
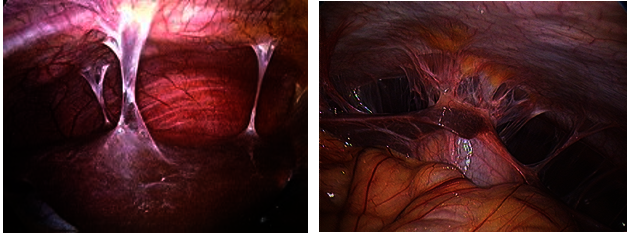
It will be easier to understand the abnormal photos below when you compare them to a normal pelvis. This photo shows a normal uterus, fallopian tubes, and ovaries.
These photos show a normal right tube and ovary (photo on the left) and a normal left tube and ovary (photo on the right). That may be confusing, we are just seeing if you are paying attention.
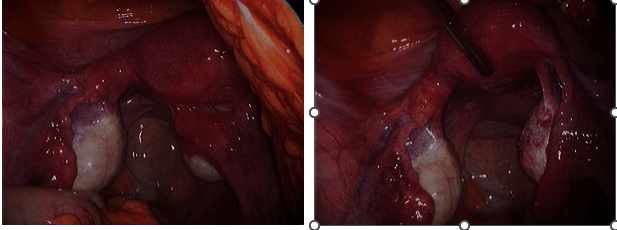
In the left photo, the right fallopian tube is stuck to the back of the uterus. The right ovary can be seen `peeking out` below the tube. In the right photo, the adhesions between the right tube and the back of the uterus have been removed and the right tube is in its normal position. The right ovary is now clearly visible.
This photo was taken during surgery 6 weeks later. The right fallopian tube has re-adhered to the back of the uterus as if nothing had ever been done. This is an example of recurrent dense cohesive adhesions.
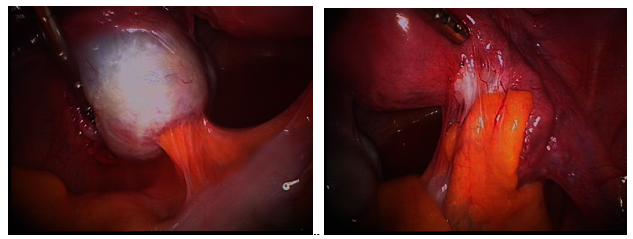
In this patient, benign tumors (dermoid) had been removed from the left and right ovaries 2 years earlier. The left photo shows the large bowel (colon) adhered (stuck) to the incision in the left ovary where the tumor was removed. The entire right ovary and fallopian tube are encased in adhesions from the colon in the right photo. A larger dermoid had been removed from the right ovary. Both ovaries had no adhesions prior to the original surgery. These are examples of denovo or new adhesions – adhesions developing in areas where there were none before surgery. Both are dense, vascular adhesions and likely to recur after they have been removed.
The left photo shows a uterus, tubes and ovaries encased in adhesions resulting from infection. The photo on the right is a closeup showing the appearance of dense vascular adhesions. Note they are more translucent than the filmy adhesions to the left and right of the center group.
The photo on the left demonstrates filmy avascular adhesions covering the left ovary. They are very translucent and contain virtually no blood vessels. These adhesions are the least likely to recur after removal. The photo on the right shows the uterus and ovaries of the same patient after all adhesions have been removed.
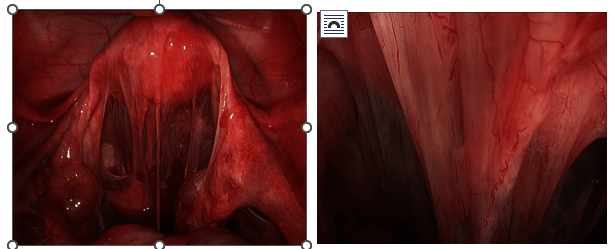
These 2 photos show Fitz-Hugh-Curtis adhesions that develop between the surface of the liver and the right side of the diaphragm. They are the result of a pelvic infection sometime in the past.
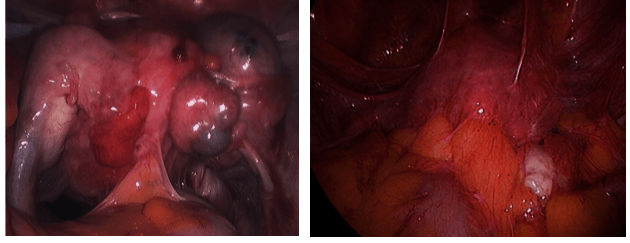
These 2 photos show a pelvis that is not reconstructible. You see no normal anatomic structures. No tubes, no ovaries, and only a hint of a uterus. These adhesions are the result of previous surgery for endometriosis. No conservative procedure has any reasonable chance of restoring normal pelvic anatomy.
If you have questions about adhesions or would like to schedule an appointment with Dr. Johns, send us the contact form on the home page.